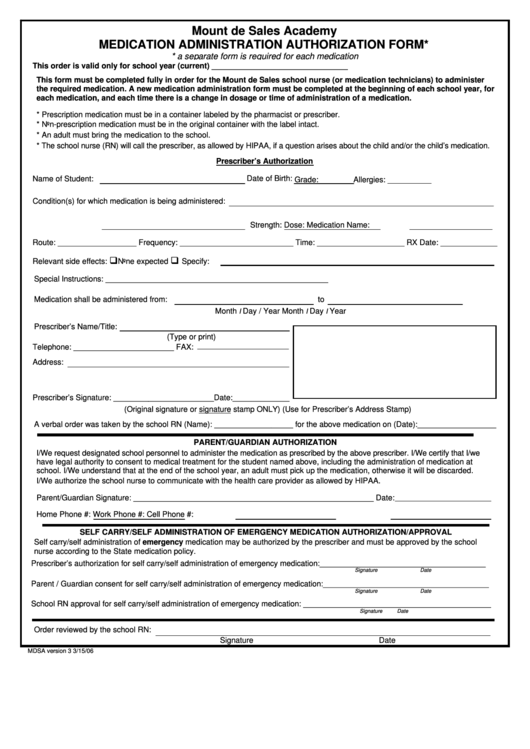
Medication Administration Authorization Form 2006 Printable Pdf Some forms cannot be viewed in a web browser's pdf viewer and must be opened in the adobe reader application on your desktop system. click here for instructions on opening this form. Submit online at: covermymeds main prior authorization forms cigna or via surescripts in your ehr. our standard response time for prescription drug coverage requests is 5 business days. if your request is urgent, it is important that you call us to expedite the request.
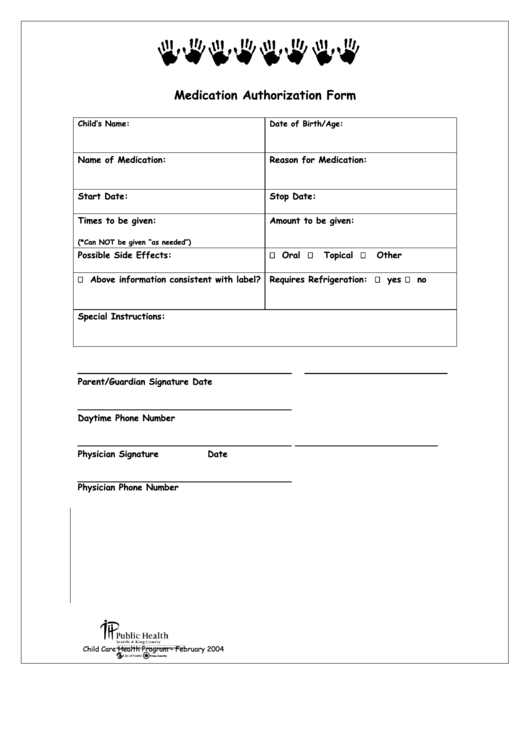
Medication Authorization Form Printable Pdf Download Documentation of an adverse event or lack of efficacy with the generic formulation and completion of an fda medwatch form. please forward a copy of the submitted medwatch form with this request. forward the original medwatch form to the fda. name: is this brand medically necessary? no. Optum rx has partnered with covermymeds to receive prior authorization requests, saving you time and often delivering real time determinations. visit go.covermymeds optumrx to begin using this free service. please note: all information below is required to process this request. mon fri: 5am to 10pm pacific sat: 6am to 3pm pacific . Easily access and download all unitedhealthcare provider forms in one convenient location. the unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals, demographic changes and more. Does the patient require a specific dosage form (e.g., suspension, solution, injection)? if so, please provide dosage form: are additional risk factors (e.g., gi risk, cardiovascular risk, age) present?.

Fillable Online Authorization For Medication Administration Form Easily access and download all unitedhealthcare provider forms in one convenient location. the unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals, demographic changes and more. Does the patient require a specific dosage form (e.g., suspension, solution, injection)? if so, please provide dosage form: are additional risk factors (e.g., gi risk, cardiovascular risk, age) present?. Prior authorization of benefits is not the practice of medicine or a substitute for the independent medical judgment of a treating physician. only a treating physician can determine what medications are appropriate for the patient. Please complete this entire form and fax it to: 866 940 7328. if you have questions, please call 800 310 6826. this form may contain multiple pages. please complete all pages to avoid a delay in our decision. allow at least 24 hours for review. is the requested medication: new or continuation of therapy?. Drug prior authorization requests supplied by the physician facility instructions: to ensure our members receive quality care, appropriate claims payment, and notification of servicing providers, please complete this form in its entirety. fax completed form to 1 888 871 0564. by using this form, the physician (or prescriber) is asking for. Instructions: please fill out all applicable sections on both pages completely and legibly. attach any additional documentation that is important for the review, e.g. chart notes or lab data, to support the prior authorization request. how did the patient receive the medication?.
